Deep brain stimulation (DBS) is a surgical procedure in which the doctor places a neurostimulator (type of device) in the brain. This then sends electrical signals to the brain regions responsible for movement, pain, mood, weight, obsessive-compulsive thoughts, and waking up from a coma.
This makes it possible to treat, among other things, Parkinson’s disease, chronic pain, and epilepsy.Deep brain stimulation is only possible when classical treatment options fail.
Although the installation of the system – which usually takes place in a few phases – is usually safe, problems sometimes arise. many patients experience relief from the original symptoms due to deep brain stimulation.
Purpose Of Deep Brain Stimulation
Deep brain stimulation can be used for patients with:
- chronic pain
- Parkinson’s disease (neurological disorder with tremors) when the symptoms are not controlled with medication. Deep brain stimulation does not cure Parkinson’s disease, but it reduces symptoms such as slow movements, difficulty walking, stiffness, and tremors (shaking).
- dystonia (uncontrolled or slow movement)
- severe depression that does not respond well to medication
- an obsessive-compulsive disorder / compulsive disorder
- epilepsy: Usually epilepsy surgery has already been performed first and only if this fails or is insufficiently effective, the patient may be eligible for deep brain stimulation.
- essential tremor (uncontrollable tremors of unknown cause)
- Tourette’s syndrome (disorder with vocal and motor tics) (rare)
- Huntington’s disease (progressive neurological disorder)
Furthermore, DBS may be useful for the treatment of severe obesity, anorexia nervosa and addiction problems, but as of September 2020, the studies are still experimental.
Contraindication Of Neurostimulator Placement In Brain
This operation is riskier in people over 70 and in patients with high blood pressure and diseases that affect the blood vessels in the brain. The surgeon must then carefully weigh the benefits of the operation against the risks. If necessary, the surgeon is able to reverse the deep brain stimulation procedure. DBS has fairly minimal absolute contraindications. 
Deep brain stimulation is contraindicated in patients who cannot operate the neurostimulator properly. Once implanted, patients with deep brain stimulators should not undergo whole-body MRI scans, transcranial magnetic stimulation, and diathermy (treatment based on heat action).
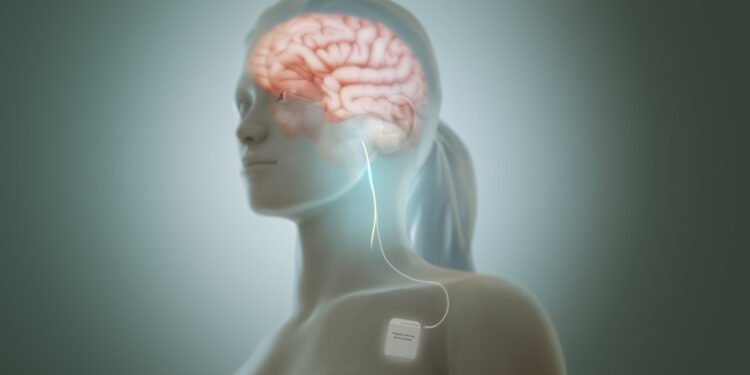
Components of the system of deep brain stimulation
The deep brain stimulation system consists of four parts:
- One or more insulated wires, leads, or electrodes, which the surgeon places in the brain
- Anchors to fix the cables to the skull
- The neurostimulator, delivers the electrical current. The simulator is similar to a pacemaker. The surgeon usually places these under the skin near the collarbone, but sometimes they also place them elsewhere in the body.
- In some patients, the surgeon inserts another thin insulated wire (an extension) to connect the cable to the neurostimulator
The surgeon performs surgery to place each component of the neurostimulator system. In adults, the placement of this system is done in one or two separate surgeries.
Before Surgery
To Investigate
The patient will have a complete physical examination. The surgeon will order many lab and imaging tests, including a CT scan or MRI scan. These imaging tests determine the exact brain region responsible for the symptoms.
The surgeon uses the images to place the lead in the brain during surgery. Sometimes the patient may also need to see a neurologist, neurosurgeon, and/or psychologist to ensure that the procedure is appropriate and has the best chance of success.
Our bodies, incredibly complex and filled with hidden details, often keep secrets that our eyes can’t see. But understanding what’s happening inside you can give you the power to make smart choices about your health. Full body scans, available at facilities like Craft Body Scan, are tools that help find issues early and support preventive healthcare.
Instead of waiting for symptoms, these scans look at your lungs, heart, abdomen, and pelvis using advanced technology. They can spot potential problems like tumors, aneurysms, and even early signs of serious diseases. Picture knowing about your current health and potential future risks – it’s a proactive way to take control of your well-being before you feel unwell.
Medication
The surgeon must be aware of any pregnancy, alcohol abuse, and any over-the-counter and prescription medications, herbs, supplements, or vitamins used. Sometimes the patient may need to temporarily stop taking blood thinners suchas warfarin(Coumadin,Jantoven), aspirin, ibuprofen, naproxen, and other NSAIDs (non-steroidal anti-inflammatory drugs). The surgeon also reports which medicines or substances the patient can still take on the day of or days before the operation. Smokers should quit smoking before surgery.
Just Before Surgery
The patient must also be fasting (not eating or drinking) eight to twelve hours before the operation. He washes the hair with special shampoo just before the surgical procedure.
During The Surgical Procedure
Phase 1
Phase 1 is usually done under local anesthesia (in children under general anesthesia). Then the surgeon shaves off a little hair on the head. The surgeon then places it in a special frame with small screws to keep the head still during the procedure.
Subsequently, the patient is given numbing medication at the place where the screws come into contact with the scalp. Sometimes the surgeon performs the procedure in the MRI machine and a frame sits on top of the head instead of around the head.
The surgeon then applies the anesthetic medication to the scalp where the surgeon will open the skin, and then drills a small opening in the skull, and places the lead in a specific brain region. When the surgeon treats both sides of the brain, he makes an opening on each side of the skull and inserts two guides.
Sometimes he has to send electrical impulses through the conductor to make sure it is connected to the brain area responsible for the symptoms. The patient may need to answer questions or describe pictures or be asked the moving legs or arms. This way the surgeon knows that the electrodes are in the right place and the expected effect is achieved.
Phase 2
Stage 2 is done under general anesthesia. The timing of this phase of the surgery depends on the location of the stimulator in the brain.
The surgeon makes a small surgical opening (incision), usually just below the collarbone, and implants the neurostimulator. Sometimes he places it under the skin in the lower breast or abdomen.
The doctor places the extension under the skin of the head, neck, and shoulder and then connects it to the neurostimulator. He then closes the incision. The device and wires are not visible outside the body.
Once connected, electrical pulses travel from the neurostimulator, along the extension wire, to the lead, and into the brain. These tiny pulses disrupt and block the electrical signals that cause symptoms of certain diseases.
After The Dbs Procedure
Usually, patients spend about three days in the hospital. The patient also takes prescribed antibiotics to prevent infection. During a follow-up visit, the surgeon activates the stimulator and adjusts the stimulation amount.
When one or more of the following signs appear, contact with the surgeon is necessary:
- numbness or tingling on one side of the body
- headache
- itching or hives
- a fever
- nausea and vomiting
- pain
- vision problems
- problems speaking
- redness, swelling, or irritation at one of the surgical sites
- muscle weakness
Prognosis Of Deep Brain Stimulation
Thanks to the operation, the symptoms improve in many patients, which increases the quality of life. Most patients still require medication but at a lower dose.
Risks
General Anesthesia
Some patients experience drug reactions or breathing problems.
Deep brain stimulation
Deep brain stimulation is a safe and effective procedure, but there are always risks involved, such as:
- concentration problems
- dizziness
- an allergic reaction to the deep brain stimulation components
- a stroke
- an infection
- a leakage of cerebrospinal fluid, possibly causing headaches or meningitis
- a loss of balance, impaired coordination, or mild loss of movement
- vision problems
- shock-like sensations
- speech problems
- temporary pain or swelling where the device is implanted
- temporary tingling in the face, arms, or legs
Furthermore, problems sometimes arise if parts of the deep brain stimulation system break or move, such as a defective device, a broken lead or broken wires, a failed battery, etc. Sometimes a new operation is required.
Brain Surgery
Possible risks of brain surgery are:
- a stroke
- a blood clot or bleeding in the brain
- a coma
- a brain swelling
- an infection in the brain, in the wound, or in the skull
- epileptic attacks
- problems with speech, memory, muscle weakness, balance, vision, coordination, and other functions, which may be short-lived or permanent
- confusion, which usually lasts for several days or weeks